Many stakeholders have shared the concerns and challenges that are occurring with patient care and the devastating impact to patients because of the closure of Michigan Pain Consultants (MPC) practices. MI-CCSI, in partnership with our content experts on treating AUD and SUD, are researching options to support this vulnerable population as well as the providers who have been put into the position of coordinating and managing the care that was previously provided by MPC. MI-CCSI has compiled some resources to assist with the immediate need.
Responding to Sudden Practice Disruption & Potential OUD Treatment Gaps
This guidance was produced by Eva Quirion, Ph.D, APRN, FNP-C. Dr. Quirion has been a longtime collaborator with MI-CCSI, bringing her experience and expertise in the treatment of pain and substance use disorders, to act as advisor and inform trainings and initiatives. In her practice, she has extensive experience in treating substance use disorders, managing tapering of controlled substances and working closely with patients and primary care providers to improve patient safety related to opioids. She is responsible for the review of controlled substances for new primary care patients at St. Joseph Healthcare in Bangor, member of the Maine Quality Counts Chronic Pain Collaborative, and member of the Community Care Partnership of Maine Controlled Substance Committee.
Based on this experience, Dr. Quirion has provided guidance on managing patients seeking alternatives to care as a result of Michigan Pain Consultants closing their practices.
Suggested guidance and benchmark in addressing the current situation occurring with patients as a result of the closing of the Michigan Pain Consultants practices
The state of Maine encountered a similar situation with the sudden disruption of care from a prescriber practice that treated a significant number of patients with Opioid Use Disorder (OUD). The Maine Prescription Monitoring Program put together a public health message that offers the following guidance.
If patients present at your clinic or ED, using best clinical judgement, please consider taking the following actions:
- Most importantly, in nearly all circumstances, we encourage providers to honor requests for buprenorphine prescription refills from individuals currently on the medication. Suddenly stopping buprenorphine involves high risk of morbidity and mortality. Maintaining current patients on buprenorphine can help keep them engaged in treatment and avoid overdose death.
- Use the Prescription Monitoring Program (PMP), Michigan Automated Prescription System (MAPS) to look up any patient requesting a buprenorphine refill.
- Remember that any prescriber with a DEA registration can now prescribe buprenorphine without restriction (since federal elimination of the DEA “X-waiver” on 1/1/23).
- Consider continuing the dose and formulation of the current prescription (verified on PMP) until a longer-term prescribing relationship can be established.
- Consider providing a 7–14-day supply. Buprenorphine is Schedule III and has low risks for established patients.
- Recommend the patient continue to use the same pharmacy to ensure higher likelihood that their prescribed formulation is available.
- Using toxicology testing is optional for short-term refills. Prescribers should know whether testing available at their facility includes buprenorphine and/or fentanyl (these are not included in many “opioid” toxicology panels). Results should be used to assist with harm reduction counselling, not to withhold treatment.
- Co-prescribe naloxone to help reduce risk of unintentional drug overdose. While naloxone is now available over the counter, writing a prescription may assist the patient in obtaining reduced cost or free naloxone, depending on insurance coverage.
- Prescribers should familiarize themselves with the risks and benefits of different buprenorphine formulations and individualize treatment as much as possible.
Additional expert opinion guidance and resources from the Maine Substance Use Disorder (SUD) Learning Community can be found here: https://mesudlearningcommunity.org/.
Additional guidance on steps to take when the patient presents to the office:
- When integrating these patients into care, prioritize patients at higher risk for adverse outcomes and address changes in these patients first. Patients at potentially higher risk could include:
- Those with Higher MME co-prescribed controlled medications (i.e., opioids and benzodiazepines).
- Patients with concurrent illnesses making these medications riskier (i.e., apnea, COPD, non-reassuring behavior with medication, history of drug misuse and more).
- Each of these patients should receive a PHQ-9 screening to assess for depression, as there are high rates of depression in those with chronic pain.
- It is highly advised to perform a suicide assessment and establish a safety plan, if needed. Some patients may feel distraught at the thought of changing their pain plan.
- It is highly recommended to conduct screening for all substance use disorders (opioids, stimulants, benzodiazepines, alcohol, etc.) using DSM-V criteria. Training and resources on conducting screening, appropriately responding to positive screens, and considerations for treatment can be found on the MI-CCSI website at: https://www.miccsi.org/training_event/sbirt-enduring-series/.
- Documentation considerations for patients on risky prescribing:
- Patients with these risks will likely need more frequent visits, more monitoring, and consideration of change in plan of care. Make sure that they have frequent office visits, or at least check-ins with care management or other support staff.
- Complete a full pain evaluation (OLD CARTS or other) as well as previous treatments, what worked, what did not, etc.
- Document daily function, ADLs, employment, care for family and home. This way, when treatment plans change, the function is already documented, and providers will not have to rely on subjective assessments while they taper (if they so choose). Ask a patient to “run me through your typical day” to determine their level of functionality. If this question is asked without telling a patient ahead of time that the prescriber is trying to assess the efficacy of the medications, they are likely to get a better picture of those who are taking lots of pills, but still not functioning.
- Lastly, if the provider feels unprepared to manage some of these patients, have readily available a way to outreach to experts, such as through OPEN at: https://michigan-open.org/programs/request-a-consultation/
The impact on this highly vulnerable patient population is not fully known at this time. The goal of this message is to bring awareness of the possible concerns of safety, mental health, and overall well-being, in the spirit of empowering providers with tools and resources.
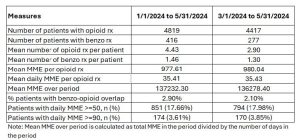
Additional input from Eva Quirion, Ph.D., APRN, FNP-C, based on review of data* presented by Chad Brummett, MD of OPEN, at most recent Coordination meeting: Michigan Pain Consultants
If we look at this group of folks in terms of risk of adverse effects if their prescriber is lost, those on combination opioid & benzodiazepines are most at risk for adverse effects. Here is how I would prioritize below:
- Higher doses of opioids & higher doses of benzodiazepines
- Any dose of opioids & any dose of benzodiazepines
- Any dose of benzodiazepines without opioids
- High dose opioid without benzodiazepines
- Lower dose opioid without benzodiazepines
Opioid withdrawal is thought of as a non-life-threatening problem, but those with a more fragile constitution and co-occurring cardiac issues (which is so often the case) may not be able to withstand the vomiting, tachycardia, and hypertension that goes along with opioid withdrawal.
Of course, benzodiazepine withdrawal can be life threatening due to risk of seizures, but again those with fragile constitution may have bad issues even without a seizure.
Lastly, those who have concurrent mental health conditions could experience destabilization and could lead to life threatening issues. For those, making sure that someone reaches them with a message of “we are taking care of you” can be reassuring and take away some of their distress.
MI-CCSI Substance Use Disorder (SUD) & Pain On-Demand Training & Resources
As part of a MDHHS grant, MI-CCSI has been compiling a resource library for care teams, to include a series of short vignettes from a number of content experts on pain management, Substance Use Disorder (SUD), and Alcohol Use Disorder (AUD). Some are currently available and more are in development and will be available late summer/early fall.
- Screening Brief Interventions and Referral to Treatment (SBIRT) – presented by Richard Brown, MD and includes seven on-demand sessions that provide key components for successfully implementing SBIRT.
- Caring for Legacy Patients with a History or Currently Receiving SUD Treatment – presented by Eva Quirion, Ph.D, APRN, FNP-C and utilizes case studies to explore treatment options and medical management considerations for chronic pain legacy patients (a patient whose care is taken over by a physician after treatment was initiated by another physician). This activity will include risk management for legacy prescriptions, (prescribing that continued beyond the usual length of time and are not discontinued after the usual recommended period) affiliated with chronic pain management.
- Challenges of Managing Pain in Patients with a History or Currently Receiving SUD Treatment – presented by Eva Quirion, Ph.D, APRN, FNP-C and includes three short on-demand vignettes that provide practical, patient-centered messaging to build comfort and confidence of the care teams.
- Substance Abuse Treatment Case Studies Series – presented by Edward Jouney, DO and includes six short on-demand vignettes that provide case studies to assist with diagnosing, monitoring and treating individuals with a history of various substance use disorders.